
John Paul Gallardo, D.D.S., P.A., Periodontics and Implant Dentistry
From Our Office
to Yours….
The management of gingival recession defects, a common periodontal condition, using root coverage procedures is an important aspect of periodontal regenerative therapy.
Tissue recession is associated with thermal and tactile sensitivity, esthetic complaints, and a tendency toward root caries.
The typical outcomes of root coverage procedures are predictable, esthetic, and at the forefront of regenerative procedures.
This current issue of The PerioDontaLetter reviews how to treat exposed root surfaces, and the most effective surgical procedures for covering them predictably.
For more detailed information on these procedures, please contact our office.
As always, we welcome your comments and suggestions.
An Update on Diagnosing and Treating Gingival Recession
Treatment of recession defects is indicated for the prevention of root caries, reducing root hypersensitivity, enhancing esthetics, augmenting keratinized tissue, eliminating inconsistency of the gingival margin, and to enhance plaque control.
The initial phase in managing gingival recession should be eliminating or correcting etiologic factors. Once the etiologic factors have been managed effectively, gingival recession can be overcome or eliminated with a variety of effective surgical modalities. Assessing periodontal support including bone levels and the height of soft tissue including interdental papilla are essential to obtaining a predictable result.
The Etiology of Gingival Recession
The anatomical factor most commonly correlated with gingival recession is a lack of, or an existing narrow band of, keratinized gingiva. Correlated anatomical features are a genetic pre-existing lack of alveolar buccal bone, high frenum pull, tooth malposition, and thin gingival phenotype.
Occlusal trauma, plaque-induced gingival inflammation and irritating oral habits may also contribute to gingival recession.


Iatrogenic factors include labial orthodontic tooth movement, which may result in the loss of the buccal alveolar plate, and pronounced buccal position of the tooth roots outside the confines of the jaw bone; crown preparations which extend too far subgingivally; impression techniques involving gingival retraction, and especially toothbrush abrasion.
Classification of
Gingival Recession
And Papilla
Dr. P.D. Miller has classified gingival recessions and loss of interproximal papilla, correlating anatomic tissue loss with the possibility of successful gingival recession treatment.
Classification of
Recession
Class I: Marginal tissue recession that does not extend beyond the mucogingival junction, with no bone loss in the interdental area, and the teeth well-aligned in the arch. With carefully performed regenerative treatment, one hundred percent root coverage can usually be anticipated.
Class II: Marginal tissue recession that extends to or beyond the mucogingival junction, with no periodontal loss in the interdental area, and the tooth/teeth wellaligned in the arch. One hundred percent root coverage can usually be anticipated.
Class III: Marginal tissue recession that extends to or beyond the mucogingival junction, with bone or soft tissue loss in the interdental area present, and malpositioned teeth. Partial root coverage can be expected.
Class IV: Marginal tissue recession that extends to or beyond the mucogingival junction, width loss of soft tissue and bone in the interdental area, and/or malpositioning of the teeth is so severe that root coverage should not be attempted. Creation of additional keratinized tissue, however, may be imperative to prevent further gingival deterioration, which could ultimately lead to tooth loss.
Classification of Papilla
Type A: No interdental bone loss, the papilla is greater than 3mm wide at its base with no loss of interdental bone, and extends 5 mm coronal to the interdental bone crest. Complete root coverage is expected.
Type B: No interdental bone loss, the papilla is less than 3mm wide at its base and extends 5mm coronal to interdental bone crest. Complete root coverage may not be possible.
Type C: Interdental bone loss, and/or the tooth is extruded, and the papilla may be greater than 3mm at its base. Complete root coverage is not expected.
The Decision Not to Treat, to Treat, and How to Treat
The decision to treat or not treat recession, and the probability of a successful outcome, can be predicted by the Miller Classifications and patient-specific factors.
In the case of recession-related root sensitivity, and if there is no concomitant esthetic complaint, a less invasive treatment is the local application of desensitizing agents.
Almost all persistent root sensitivity is caused by acids in the diet. Analysis of acids in foods and drinks is indicated.
A 5000ppm prescription fluoride toothpaste used twice a day will often improve sensitivity.
Surgical Procedures
The ultimate goal of treating a
recession defect is complete root
coverage with soft tissue, with an
esthetic appearance equal to or
approximating the adjacent soft
tissues and minimal probing depth.
Three basic surgical procedures
are used in the treatment of recession
defects:
- Free soft-tissue autografts,
allografts and xenografts
- The free gingival graft
- The subepithelial connective
tissue graft - The xenograft derived from a
species that is not human,
often porcine.
- Pedicle soft-tissue autografts
- Coronally positioned flaps
- Rotational flap procedures,
such as the lateral sliding flap.
- Soft-tissue graft procedures in combination with regenerative procedures, which may include the use of barrier membranes and chemical stimulators such as enamel matrix derivatives.
Coronally advanced flaps and lateral sliding flaps are beneficial because there is no need for palatal or other harvest sites.
Consequently, post-operative pain and attendant complications are minimized.

The Tunnel Technique
The unique characteristic of tunneling procedures for root coverage, also known as the supraperiosteal envelope technique, is that a tunnel is created keeping the interdental papillae intact. The tunnel starts from the apical approach through a pinhole, with a minimal opening incision and/or accessing coronally through the sulcus.
A connective tissue graft, acellular dermal matrix graft, or a collagen membrane is then placed in the tunnel.
The absence of vertical incisions tends to produce better esthetics and less discomfort.
Predictable Root Coverage
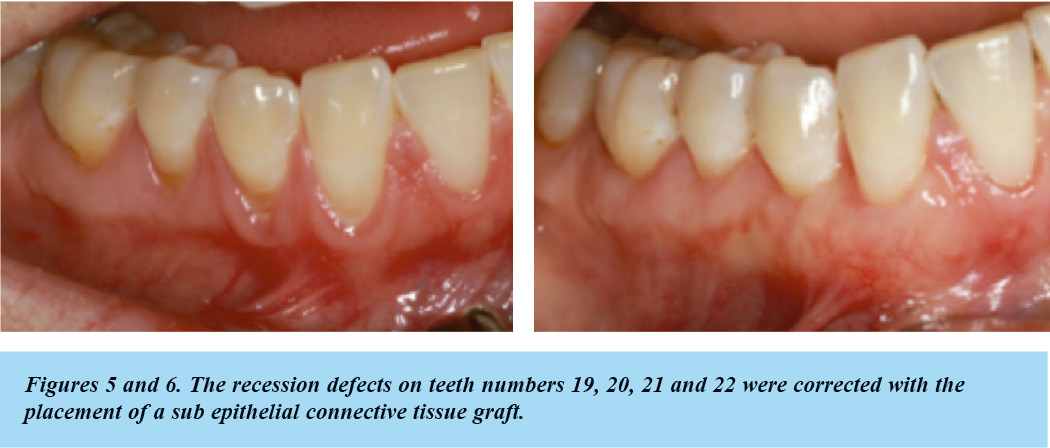
Predictable root coverage is possible for single-tooth and multiple-tooth recession defects, with subepithelial connective tissue graft procedures providing the most predictable root coverage outcomes.
For Miller Class I and II singletooth recession defects, subepithelial connective tissue graft procedures provide the most predictable results.
These results may be enhanced by the use of enamel matrix derivative and/or platelet derived growth factor (PDGF).
The subepithelial connective tissue graft, enamel matrix derivative in conjunction with the coronally advanced flap, and the acellular dermal matrix graft provide longterm predictable root coverage.
Sub-epithelial connective tissue grafting, acellular dermal matrix grafting, and xenogeneic collagen matrix-based procedures increase the density of the underlying connective tissue, and may add to the width of keratinized tissue and more predictable root coverage.
The subepithelial connective tissue graft provides superior longterm root coverage stability.
Root Preparation
Exposed roots may exhibit surface changes, including necrotic cementum and softened dentin, resulting in the need for mechanical or chemical root biomodification, which can improve the predictability of root coverage and enhance the results of root coverage procedures.
Such root preparation may include mechanical root planing or chemical conditioning of the root surface.
The resultant demineralized root surface/s creates a more favorable environment, which enhances the predictability of root coverage.
Wound Healing
Most gingival augmentation procedures result in the formation of a long junctional epithelium and connective tissue attachment with fibers parallel to the root surface. In addition, these procedures may result in the regeneration of lost alveolar bone.
Conclusion
There are a wide variety of possible mucogingival grafting techniques to correct recession defects.
These procedures are quite predictable and have minimal postoperative sequale, while producing satisfactory and predictable solutions to root recession defects.