Have you ever brushed off a nagging toothache, assuming it would go away on its own? While dental pain might seem minor at first, ignoring it could lead to more than just a trip to the dentist—it could result in serious health complications that affect your entire body.
A tooth infection doesn’t just stay confined to your mouth. In some cases, it can spread through the bloodstream, leading to dangerous outcomes like sepsis, heart complications, or even neurological damage. Keep reading to find out how your oral health could be the key to your overall well-being.
Can a Tooth Infection Affect Your Whole Body?
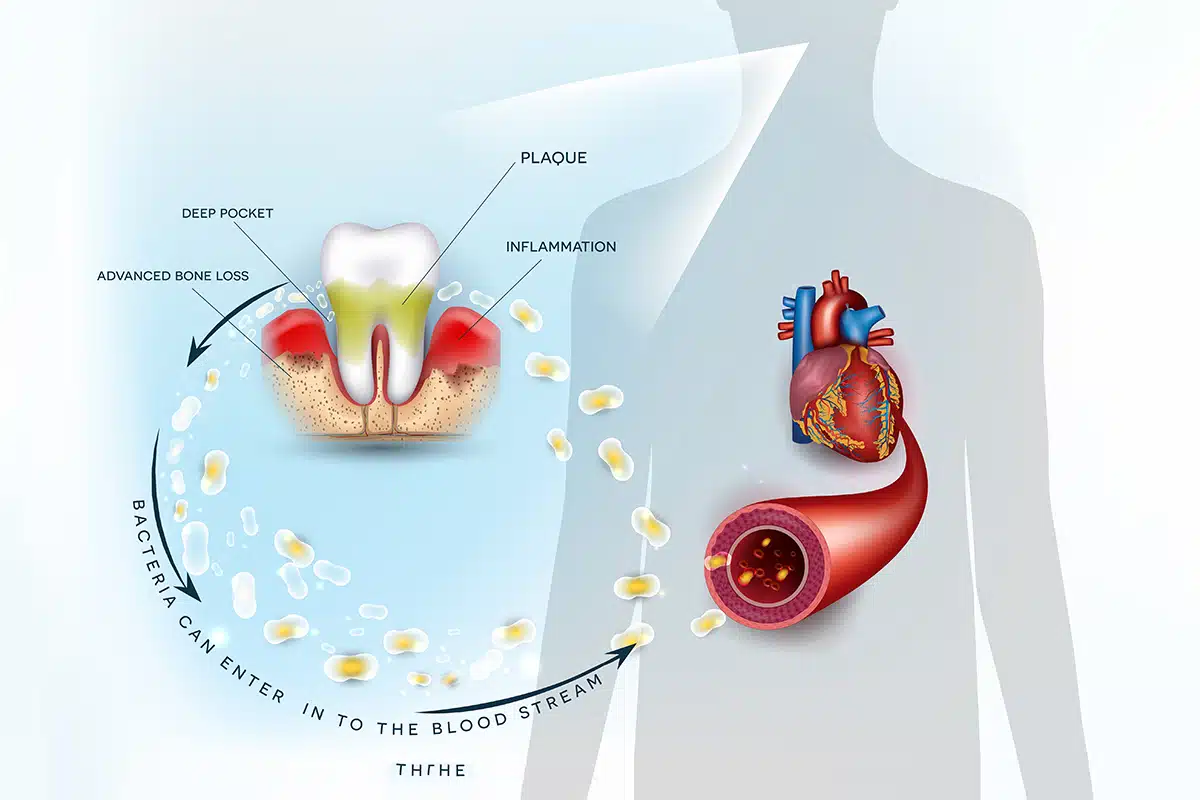
Yes, a tooth infection can spread beyond the mouth and affect the entire body. If left untreated, bacteria from the infection can enter the bloodstream, traveling to vital organs and potentially causing life-threatening conditions such as sepsis or endocarditis. This is why early diagnosis and prompt treatment are crucial—not only for saving your tooth but also for protecting your health overall. Understanding the symptoms of a spreading tooth infection can help you take action before it’s too late.
Signs and Symptoms of Tooth Infection Spreading to the Body
When a tooth infection begins to spread beyond the root of the tooth, the body often sends out distress signals in the form of symptoms that shouldn’t be ignored. These signs can manifest subtly at first, but they may rapidly intensify as the infection moves through the bloodstream and into other systems.
Recognizing these symptoms early is crucial for preventing dangerous complications. In the sections below, we’ll break down the various ways your body might be telling you that a dental infection is becoming a systemic threat.
General Symptoms
As a tooth infection begins to spread beyond its original site, the body often responds with generalized symptoms that resemble those of the flu or a common illness. These signs are your body’s way of signaling that something more serious may be going on internally. Don’t overlook these early warning signs:
- Fever
- Chills
- Fatigue
- Malaise
- Headache
- Muscle aches
Facial and Oral Symptoms
As the infection worsens, it often becomes more visible and painful in the face and mouth area. These symptoms can interfere with basic activities like eating, speaking, or even opening your mouth, and should be considered red flags for a spreading infection:
- Swelling of the face, cheeks, or jaw
- Pain that radiates to the ear, jaw, or neck
- Bad breath
- Pus draining from the gums
- Difficulty opening or closing the mouth
- Difficulty swallowing
Gastrointestinal Symptoms
When an infection spreads, it doesn’t just stay in one part of the body—it can also affect the digestive system. These gastrointestinal symptoms might not immediately make you think “tooth infection,” but they’re often linked to systemic inflammation and the body’s immune response:
- Nausea
- Vomiting
- Diarrhea
- Abdominal pain
Cardiovascular Symptoms
Once an infection reaches the bloodstream, it can impact the cardiovascular system in serious ways. The symptoms listed below are indicators that the infection may be placing stress on your heart and circulation—conditions that require immediate medical attention:
- Rapid heart rate
- Low blood pressure
- Shortness of breath
Neurological Symptoms
Though less common, a spreading dental infection can occasionally impact the nervous system. These neurological symptoms may appear in more advanced stages and should never be ignored, as they could point to serious systemic involvement or even infection in the brain:
- Confusion
- Seizures
- Numbness or tingling in the face or limbs
Other Symptoms
While these symptoms may not be as common, they can still occur in some cases and are worth being aware of—especially if they appear alongside more classic signs of infection. They may indicate that the infection is taking a toll on other systems in the body:
- Joint pain
- Skin rash
- Weight loss
Causes and Risk Factors of Dental Infections
Understanding what causes a dental infection—and who is more likely to develop one—is key to preventing serious complications. Several factors can increase your risk, from everyday habits to underlying health conditions. Here are some of the most common causes and risk factors that could set the stage for an infection:
- Poor Oral Hygiene: Not brushing or flossing regularly allows plaque and bacteria to build up, increasing the risk of cavities and infections.
- Bacterial Invasion: Bacteria can enter the tooth through cracks, cavities, or gum pockets, leading to inflammation and infection.
- Tooth Decay: Advanced decay can penetrate the enamel and reach the pulp, where infection can take root and spread.
- Trauma: Cracks or chips from injuries can expose the tooth’s inner tissues to bacteria.
- Wisdom Teeth: Impacted or partially erupted wisdom teeth are prone to infection due to difficulty cleaning them properly.
- Weakened Immune System: Conditions like diabetes or autoimmune diseases can impair the body’s ability to fight off infection.
- Smoking: Tobacco use weakens the immune system and damages gum tissue, making infections more likely and harder to treat.
- Bad Diet: Diets high in sugar and low in essential nutrients can feed harmful bacteria and impair the body’s defenses.

Complications of an Untreated Abscess
Ignoring a dental abscess can have far-reaching consequences beyond tooth loss. When bacteria from an untreated infection spread, they can affect vital organs and systems, leading to serious—even life-threatening—health conditions. Understanding these complications underscores the importance of seeking treatment early before the infection has a chance to escalate.
Gum Disease
When left untreated, a tooth abscess can contribute to or worsen periodontal disease. This condition affects the gums and supporting structures of the teeth, potentially leading to tooth loss and bone damage. Gum disease also increases the risk of systemic issues, making it more than just a local oral health concern.
Ludwig’s Angina
This rare but serious complication is a type of cellulitis that affects the floor of the mouth and neck. Caused by a spreading dental infection, Ludwig’s angina can lead to difficulty breathing or swallowing and requires emergency treatment to prevent airway obstruction.
Dental Cysts
An untreated abscess can result in the formation of a dental cyst—an enclosed sac filled with fluid or pus near the tooth root. While sometimes harmless, cysts can become infected or grow large enough to cause discomfort, damage to the jawbone, or displacement of nearby teeth.
Sepsis
Sepsis is a life-threatening reaction to infection that occurs when the body’s immune response causes widespread inflammation. A dental abscess that enters the bloodstream can trigger this dangerous condition, leading to organ failure or death if not treated promptly in a hospital setting.
Osteomyelitis
Osteomyelitis is a serious bone infection that can result from bacteria spreading from a dental abscess. It most commonly affects the jaw and can lead to persistent pain, swelling, and destruction of bone tissue. Treatment often requires antibiotics and, in some cases, surgical intervention.
Endocarditis
Endocarditis is an infection of the inner lining of the heart chambers and valves, often caused when bacteria from a dental infection enter the bloodstream. People with preexisting heart conditions are especially at risk. This complication can be life-threatening and demands immediate medical care.
Before & After Photos


* All patients are unique and individual results may vary.
Available Treatments for a Dental Abscess
Treating a dental abscess requires swift and targeted intervention to eliminate the infection and prevent further complications. Depending on the severity and spread of the infection, treatment may involve medication, surgical procedures, or both. Below are some of the most common and effective approaches used by dental professionals today.
Antibiotics
Antibiotics are often the first line of defense when treating a dental abscess, especially if the infection has started to spread. They help eliminate the bacterial infection and reduce inflammation. While they won’t fix the root problem, antibiotics are essential for stabilizing the patient before any further dental procedures.
Apicoectomy
An apicoectomy is a surgical procedure used when a standard root canal isn’t enough to remove the infection. It involves removing the tip of the tooth’s root and sealing it to prevent reinfection. This treatment is often recommended when an abscess persists after previous endodontic therapy.
Drainage
In some cases, draining the abscess is necessary to relieve pressure and remove pus from the infected area. This procedure is typically performed under local anesthesia and provides immediate relief from pain. Drainage is often combined with antibiotics and other dental treatments to fully resolve the infection and prevent recurrence.
Treatment of sepsis
When a dental infection progresses to sepsis, it becomes a medical emergency. Treatment typically involves hospitalization, intravenous antibiotics, and supportive care to stabilize blood pressure and organ function. Prompt intervention is critical, as sepsis can escalate rapidly and result in serious long-term consequences or death if not addressed immediately.
Root canal treatment
Root canal therapy is a common and effective way to treat a dental abscess when the infection is confined to the tooth. During this procedure, the infected pulp is removed, the inside of the tooth is cleaned and sealed, and a crown is usually placed for protection. It saves the natural tooth and prevents future infections.
Choosing a Dentist for Your Treatment
Treating a dental abscess isn’t just about relieving pain—it’s about preventing long-term complications. That’s why it’s so important to trust your care to a seasoned professional. An experienced dentist understands how to identify the earliest signs of a spreading infection and provide targeted treatment to protect your overall health.
At Gallardo Periodontics and Implant Dentistry, Dr. John Paul Gallardo, DDS, PA, brings more than 25 years of specialized experience in periodontics and implant dentistry. Recognized as one of South Florida’s top periodontists, Dr. Gallardo combines advanced technology with a compassionate approach to ensure effective and comfortable care. Call us today at 305-447-1447 or visit our contact page to schedule your consultation.
